Burns are a global public health problem. This is due to the high
rate of burn mortality and morbidity, especially in low- and
middle-income countries, where more than 95% of the incidence of burns
causes death (mortality). However, death is not the only consequence of
burns. Many burn patients eventually experience disability (morbidity).
This often creates a stigma against community rejection. (Ziaeian,
Boback and Gregg C. Fonarow. (2016).)
Burns (combustio) are tissue
loss caused by contact with heat sources such as water, fire,
chemicals, electricity, and radiation. Burns will cause not only skin
damage, but also affect the entire body system (Brunner & Suddarth,
2014)
Burns are a form of tissue damage and or loss caused by
contact with sources that have very high temperatures (eg fire, hot
water, chemicals, electricity, and radiation) or very low temperatures.
Upon contact with a heat source (or other cause). A chemical reaction
takes place that drains energy from the tissue so that the cell is
reduced and damaged (Moenadjat 2014)
Burns are damage to body
tissues, especially the skin as a result of direct or intermediary with
chemical, electrical, and radiation heat sources. Burns are wounds
caused by heat trauma which give symptoms depending on the area and
location of the wound (Brunner & Suddarth, 2014)
Nursing Assessment
Assessment
of patients with burns is intended to collect the latest data and
information about the patient's status, with the assessment of the
Iitegument system as an assessment priority. Systematic assessment of
the patient includes a history specifically related to difficulty
moving, palpitations. Each symptom should be evaluated for its time and
duration as well as its precipitating factors.
1) Client identity. In addition to the client's name, age, gender, religion, occupation and education.
2)
Activity/rest. Signs: decreased strength, resistance, limited range of
motion in the affected area, impaired muscle mass, changes in tone.
3)
Circulation. Signs: hypotension (shock), decreased peripheral pulse
distal to the injured extremity, generalized peripheral vasoconstriction
with loss of pulse, white and cold skin (electrical shock),
tachycardia, dysrhythmias, tissue edema formation.
4) Ego
integrity. Symptoms: problems with family, work, finances, disability.
Signs: anxiety, crying, dependence, denial, withdrawal, anger.
5)
Elimination. Signs: decreased/absent urine output during the emergency
phase, color may be reddish black in the presence of myoglobin,
indicating deep muscle damage, diuresis (after capillary leakage and
mobilization of fluid into the body circulation), decreased bowel sounds
are absent.
6) Food or liquid. Signs: generalized tissue oedema,
anorexia, nausea/vomiting. Symptoms: decreased appetite, bowel sounds
and decreased intestinal peristalsis, changes in bowel habits.
7)
Neurosensory. Symptoms: border area, tingling. Signs: changes in
orientation, affect, behavior, decreased deep tendon reflexes in
extremity injuries, seizure activity, corneal laceration, retinal
damage, decreased sharpness vision.
8) Pain/comfort. Symptoms:
various pains, e.g., first degree burns are extremely sensitive to
touch, pressure, air movement, and temperature changes.
9)
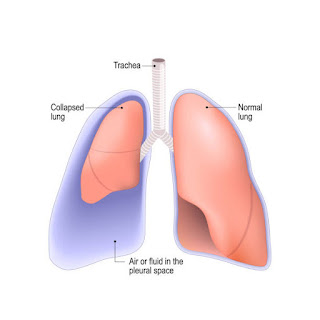
Breathing. Symptoms: confined in an enclosed space, prolonged exposure
(possible inhalation injury). Signs: shortness of breath, coughing
wheezing, carbon particles in sputum, inability to swallow oral
secretions and cyanosis, indications of inhalation injury. Thoracic
expansion may be limited to the presence of burns to the chest
circumference, airway or stridor/wheezing (obstruction related to
laryngospasm, laryngeal edema), breath sounds: deep airway secretions
(rhonchi).
10) Security. Signs: generalized skin: deep tissue
instruction may not be evident for 3-5 days in connection with the
process microvascular thrombus in some wounds.
11) Medical history
- Chief complaint: infection in burns
- History
of present illness: Most or most of the causes of burns are due to
electric shock, heat, temperature, chemical mediators.
- Past medical history: the client does not have a history of previous illnesses related to burns.
- Family history of disease: no case correlation on family members to the incidence of burn infection. (Price, A. Sylvia 2014)